The Importance of Accreditation in the Whole Body Donor Industry

This video explores the difference between accreditation and non-accreditation and why choosing an AATB-accredited organization is important when researching whole body donation.
Breaking the Code: Unmasking Your Health Secrets with Biomarker Testing
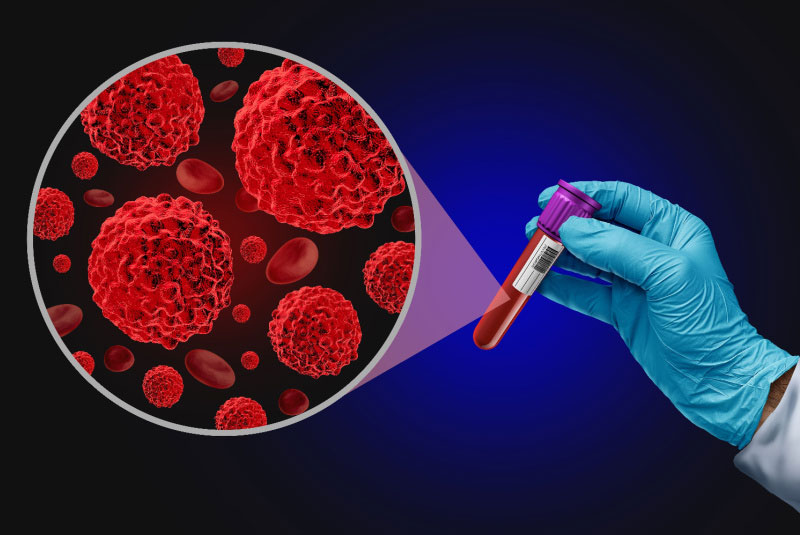
Biomarker testing has emerged as a revolutionary tool in modern medicine, offering the potential to revolutionize cancer diagnosis and treatment strategies. This comprehensive approach aids in providing personalized treatment plans and monitoring the effectiveness of interventions, enhancing patient outcomes.
Some Compelling Reasons to Consider Donating your Body to Science

Anatomical donation is an alternative to traditional funeral arrangements with the potential to impact the quality of medical care and breakthroughs for generations to come.
The Extraordinary Symphony of Deep Brain Stimulation

Deep brain stimulation (DBS) is a groundbreaking surgical therapy that has revolutionized the treatment of neurological disorders such as Parkinson’s disease, dystonia, essential tremor, epilepsy, Tourette syndrome, and obsessive-compulsive disorder. It is also being studied as a potential treatment for chorea, chronic pain, cluster headaches, dementia, depression, addiction, and obesity.
Exploring the Compassionate World of Hospice Care

Hospice is a vital part of healthcare with this compassion-driven type of care focusing on end-of-life care versus curing and prolonging life. Their end-of-life care includes emphasis on personalized care plans, managing symptoms and pain, improving quality of life, assisting with emotional, psychosocial, and spiritual aspects of death, providing supplies and equipment, helping teach families how to care/interact with the patient, and delivering special services including physical therapy or music and art therapy.
The Neurological Impact of Grief

While losing a loved one is a universal experience, the intensity of loss can impact every individual emotionally and/or physically. Traumatic loss can come in many forms including serious illness or death of a loved one and the brain commonly responds similarly to emotional trauma or PTSD.
Global Goodbyes: Celebrating Life Through Funeral Traditions

Mourning and honoring the deceased is never one size fits all and the beauty in death is the unique variety of life celebrations and how people honor their deceased loved ones.
Sudden Cardiac Arrest Awareness Month: Empowering Education for Lifesaving Knowledge

The month of October is National Sudden Cardiac Arrest Awareness Month, which is dedicated to educating the public about what sudden cardiac arrest is and how to properly respond. To be clear, sudden cardiac arrest is not a heart attack.
Protecting Our Mind: Where We Stand Against Our Fight With Alzheimer’s

Sometimes, the fight against Alzheimer’s can feel endless. Still, with dedicated research and studies, the medical community is making visible strides to help manage the disease and help those affected improve their quality of life.
The Beat Goes On: Prioritizing Heart Health

“If the home is a body, the table is the heart, the beating center, the sustainer of life and health.” – Shauna Niequist Beating 2.5 billion times over the average lifetime, the heart is a vital organ with a 24/7 job, pumping blood and providing oxygen and nutrients to your body that are needed to



